Military Veterans and Depression: Guide to Treatment Options
Published:
Dec 19, 2024
,
12:37 p.m.
ET

Depression rates are notable in active-duty military and Veterans. Some of the most common leading factors of this mental health condition among those groups include age, combat and separation. Unfortunately, depression can be challenging to diagnose in some Veterans.
Some individuals might fear seeking treatment due to being seen as weak or emotional. Others might fear that their military career could be affected by their mental health challenges.
Treatment is not a sign of weakness. Therapy can be discreet and confidential. This in-depth guide explores depression in the military, including warning signs and care options.
How common is depression in Veterans? Rates and trends
Rates of depression are significant in active-duty military (23%) and Veterans (20%), according to a meta-analysis study in 2021. Another study found that 11% of Veterans struggle with severe depression. In addition, the prevalence of suicidal ideation and attempts in the military was found to be around 11%.
Experts see stressful events and genetics are two leading causes of depression. Also, health problems stemming from war and combat can lead to depression. Most Veterans who struggle with depression need treatment. Fortunately, it can be a treatable mental health condition.
How is depression diagnosed in Veterans and active-duty military members?
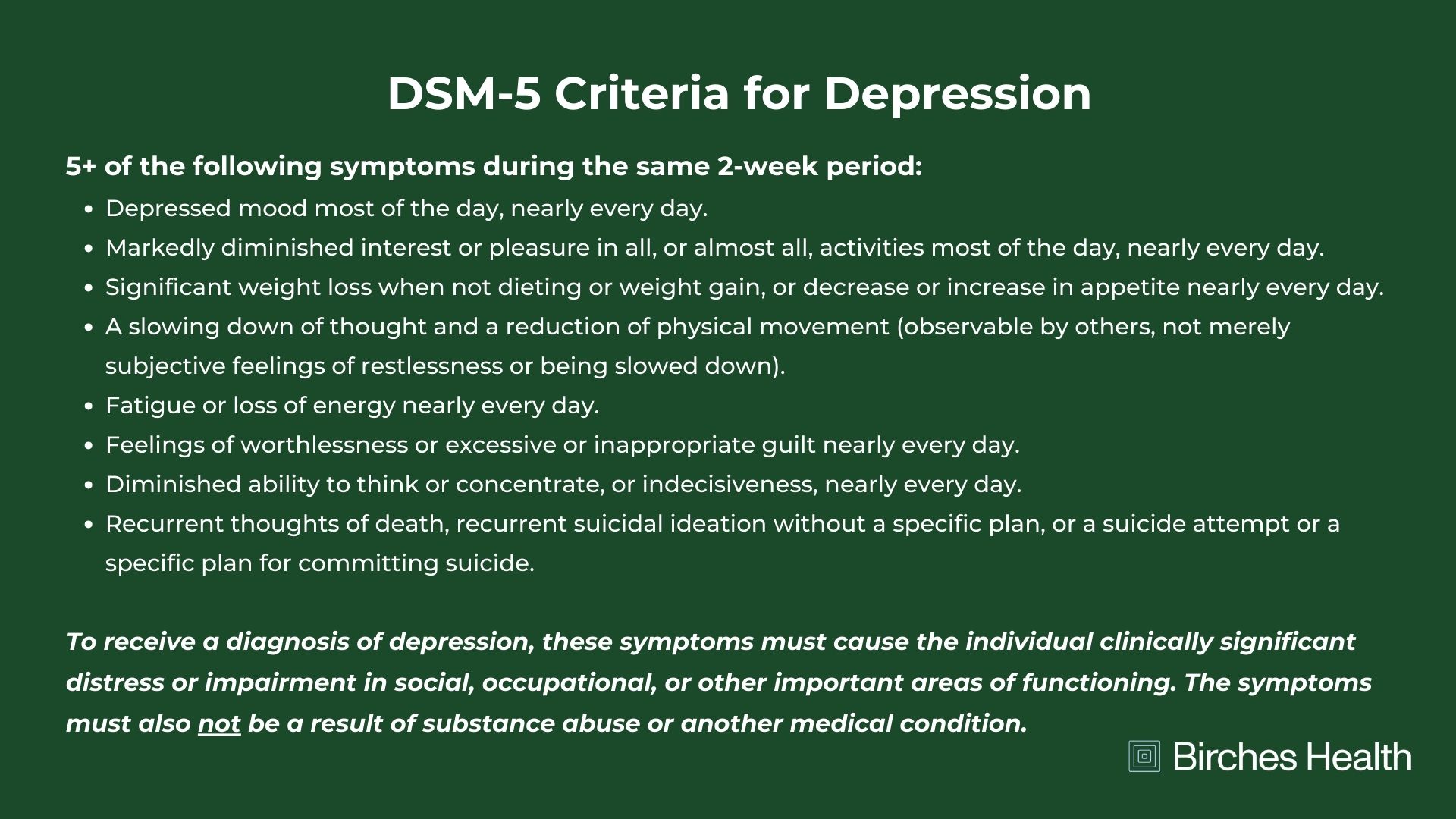
Depression is diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Veterans are evaluated under the same criteria as the general population. To receive a diagnosis, patients must meet at least five of the common symptoms of depression over the past two weeks or more within one month.
This diagnosis will also determine how the depression affected the service member’s ability to perform their military duties. From there, the patient will receive treatment for their depressive disorder. A comprehensive, custom treatment plan is recommended for successful recovery.
How can depression be treated? Understanding care options
Depression can be treated in a multitude of ways. Some of the most common options include psychotherapy, medication and lifestyle changes. The proper treatment plan depends on the severity of the condition and the patient’s preferences. Treatment options can also be combined with one another as an effective hybrid care plan.
Psychotherapy
Psychotherapy is another name for talk therapy, and it’s a standard way of treating depression. Each session helps patients overcome their negative thoughts and develop or improve their coping skills. The goal is that over time they’ll be equipped with the tools to handle daily stress and triggers.
There are different types of psychotherapy, including psychodynamic, behavioral therapy, cognitive behavioral therapy (CBT), interpersonal therapy (IPT), mindfulness-based cognitive therapy (MBCT), humanistic therapy and motivational interviewing (MI). A therapist will likely conduct an evaluation first to determine which type or combination or methods would be most effective for you personally.
CBT is a commonly used form of talk therapy for mild depression. It can be an effective method because it allows individuals to understand their negative thoughts and behaviors. Patients cultivate a sense of self-awareness to help reduce the chances of depressive periods.
Virtual Therapy
Virtual therapy is simply the digital telehealth version of psychotherapy. Although some Veterans may prefer a face-to-face option in person, others like the flexibility and ease of virtual treatment from the comfort of home. Birches Health offers treatment for depression, anxiety and behavioral addictions (gambling, sex, porn, video games, social media, etc.) from specially trained counselors. Plus, Birches is in-network with TRICARE and all other major insurance companies, so out-of-pocket costs can be low or $0. Individuals seeking care are connected with a licensed clinician who's been certified in treating that specific form of mental health challenge.
Treatment starts with a self-assessment. From there, the individual will receive an individualized treatment plan that can be implemented virtually from the safety and privacy of their home.
Getting started with Birches:
You can also feel free to call 833-483-3838
Or email help@bircheshealth.com to get in contact with the Birches team right away
Medication
Medication is mainly used to treat major depressive disorder. In addition, individuals who struggle with anxiety, bipolar disorder, borderline personality disorder or psychosis might also benefit from medication. In this case, they may be treated with a combination of antidepressants and antipsychotic drugs, known as mood stabilizers.
Antidepressant medication is prescribed when other treatments haven’t worked. There are many different FDA-approved antidepressants. This decision can only be made after an assessment and official diagnosis. While antidepressants can help most patients feel better, it can take time for them to work. Some patients might experience side effects, most of which are temporary.
Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed for depression. You might have heard of the brands Prozac, Zoloft or Celexa. SSRIs are less likely to cause side effects compared to some other antidepressants. They increase the serotonin levels in the brain, which can improve mood. As always, you should speak with your doctor about finding the right prescription for you.
Warning signs of depression in military members
It’s essential to be aware of the warning signs before they worsen. Depression can affect people differently. The signs aren’t always noticeable at first. Warning signs of depression in military members can include the following:
Appetite changes: Extreme weight gain or loss due to unhealthy or disordered eating habits.
Cognitive issues: Difficulty remembering important details, making decisions, or concentrating during work, school, or conversations.
Combat stress: Experiencing PTSD or panic attacks from traumatic events.
Decreased energy levels: Feeling a lack of energy, struggling with chronic exhaustion, or sleeping in more as a result of depression.
Loss of interest: Decreasing interest in hobbies and social activities that were once enjoyable.
Mood swings: Experiencing negative thoughts or emotions or feeling empty or hopeless for no reason.
Physical signs: Unexplained headaches, nausea, and general aches or pains.
Suicidal thoughts: Wondering whether life is worth living or wanting to die.



